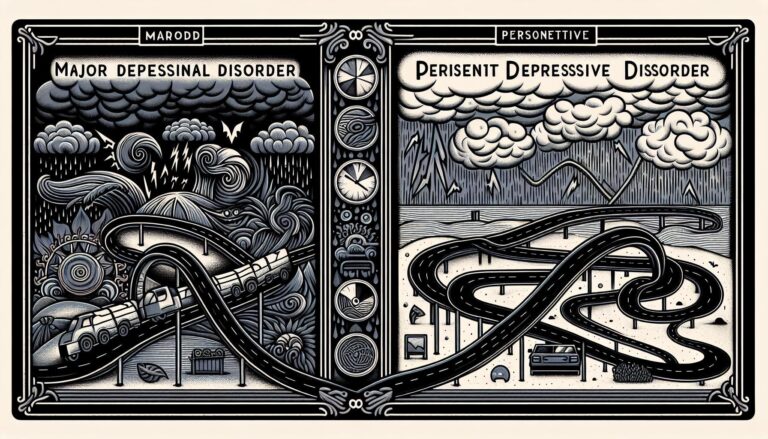
Difference Between MDD and Persistent Depressive Disorder lies in their duration and severity. Major Depressive Disorder (MDD) features intense symptoms occurring in episodes, while Persistent Depressive Disorder (dysthymia) presents a chronic, milder form of depression lasting at least two years.
Understanding Major Depressive Disorder and Persistent Depressive Disorder
Major Depressive Disorder (MDD) and Persistent Depressive Disorder (PDD), also known as dysthymia, are two significant forms of depression that affect millions of people worldwide. The primary difference between these two conditions lies in their duration and intensity. MDD is characterized by severe symptoms that hinder daily functioning and can last for weeks or months. In contrast, PDD is a chronic form of depression, typically emerging earlier in life and persisting for longer periods—often years. Individuals with PDD may experience milder depressive symptoms, but the protracted nature of this disorder can result in profound impacts on overall quality of life. Understanding the nuances in the difference between MDD and Persistent Depressive Disorder is crucial for effective diagnosis and treatment.
Another vital aspect to consider is the symptomatology associated with each disorder. While both conditions can include feelings of hopelessness, fatigue, and a lack of interest in daily activities, the specific characteristics may vary. For instance, individuals with MDD are more likely to experience intense episodes of despair, suicidal thoughts, or feelings of worthlessness, whereas those with PDD may have a more persistent sense of gloom without the episodic peaks of MDD. Recognizing these distinctions can significantly aid clinicians and patients alike in navigating the complexities of depressive disorders; thus, being informed of the difference between MDD and Persistent Depressive Disorder is essential for anyone seeking to comprehend these mental health conditions.
| Aspect | MDD | PDD |
|---|---|---|
| Duration | Short-term (weeks/months) | Long-term (years) |
| Intensity | Severe symptoms | Milder, chronic symptoms |
| Onset | Can occur at any age | Typically early in life |
| Treatment | May require urgent intervention | Long-term management needed |
Key Symptoms That Differentiate MDD from PDD
When distinguishing between Major Depressive Disorder (MDD) and Persistent Depressive Disorder (PDD), several key symptoms emerge that highlight their differences. MDD is characterized by episodic episodes of intense depressive symptoms, including:
- Loss of interest or pleasure in nearly all activities
- Significant weight changes or appetite disturbances
- Insomnia or hypersomnia nearly every day
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt
In contrast, PDD, previously known as dysthymia, is defined by a chronically depressed mood lasting for most of the day, for more days than not, over a period of at least two years. The symptoms are often less severe but more enduring, including:
- Low self-esteem
- Feelings of hopelessness
- Difficulty concentrating or making decisions
- Poor appetite or overeating
- Chronic fatigue
In terms of their impact on functioning, MDD can cause significant disruption in daily life during depressive episodes, while PDD may create a pervasive sense of sadness that quietly influences someone’s life over the years. Understanding the difference between MDD and Persistent Depressive Disorder is crucial for effective treatment and support.
The Duration of Symptoms: A Critical Distinction
The duration of symptoms forms a crucial aspect when discussing the Difference Between MDD and Persistent Depressive Disorder. Major Depressive Disorder (MDD) is characterized by episodes of significant depressive symptoms that last for at least two weeks. These episodes can be recurrent, meaning individuals may experience several bouts of depression throughout their lifetime. Symptoms can be intense and debilitating during these episodes, but they often clear up, sometimes allowing individuals to return to their normal state of functioning between episodes. On average, the duration of each episode can vary widely, spanning from a few weeks to several months, depending on various factors, including treatment and personal circumstances.
In contrast, Persistent Depressive Disorder (PDD), historically known as dysthymia, is marked by a definable set of symptoms that persist for at least two years in adults (one year in children and adolescents). While the symptoms of PDD may be less severe than those of MDD, they tend to be chronic, making the Difference Between MDD and Persistent Depressive Disorder significant in terms of duration and impact on quality of life. Individuals with PDD often find it challenging to maintain a sense of normalcy, as their depressive state can be unyielding and infiltrate various aspects of their daily lives.
| Criteria | MDD | PDD |
|---|---|---|
| Duration of Symptoms | 2 weeks or more | 2 years or more |
| Severity of Symptoms | Can be severe | Typically less severe |
| Nature of Episodes | Recurrent | Chronic |
| Functional Impact | Variable | Consistent disruption |
Difference Between MDD and Persistent Depressive Disorder in clinical settings. By acknowledging the duration and nature of symptoms, mental health professionals can tailor treatment plans that address both immediate needs and long-term management strategies for individuals struggling with these conditions.
Causes and Risk Factors for MDD and PDD
Understanding the causes and risk factors associated with Major Depressive Disorder (MDD) and Persistent Depressive Disorder (PDD) is essential for anyone looking to grasp the Difference Between MDD and Persistent Depressive Disorder. Various elements can contribute to the development of these conditions, often intersecting with each other. Some primary causes include:
- Genetics: A family history of depression often increases susceptibility.
- Biochemical Factors: An imbalance of neurotransmitters like serotonin and norepinephrine.
- Environmental Influences: Stressful life events, trauma, or a history of abuse.
- Chronic Illness: Living with a debilitating health condition can exacerbate depressive symptoms.
In considering the Difference Between MDD and Persistent Depressive Disorder, it’s important to note the role of individual risk factors that may heighten the vulnerability to either disorder. For instance, while MDD can occur in response to specific stressors, PDD often emerges when individuals have a pervasive sense of inadequacy or hopelessness. Key risk factors include:
- Age: Younger individuals are often more prone to MDD, while older adults may experience PDD.
- Gender: Women are statistically more likely than men to experience both disorders.
- Substance Abuse: A significant relationship exists between addiction and these depressive forms.
- Personality Traits: Low self-esteem or a tendency towards pessimism can elevate the risk.
Impact on Daily Life: MDD vs. PDD
The experience of living with Major Depressive Disorder (MDD) and Persistent Depressive Disorder (PDD) can greatly influence daily functioning and quality of life. Individuals with MDD may encounter intense, overwhelming episodes of depression that significantly interfere with their everyday activities. This can manifest as:
- Difficulty concentrating: Making decisions or focusing on tasks becomes an arduous challenge.
- Social withdrawal: A retreat from social interactions and previous interests, leading to isolation.
- Physical symptoms: Issues such as fatigue or changes in appetite and sleep patterns may occur.
In contrast, those coping with PDD endure a more chronic and less intense depressive state that persists for years, often making it harder to pinpoint and address. This ongoing low mood can lead to a sense of hopelessness, reflected in different daily realities, such as:
- Lowered motivation: Feeling constantly unmotivated affects work performance and personal ambitions.
- Long-term relationship strain: Continuous depressive symptoms can lead to misunderstandings and frustration with loved ones.
- Reduced overall satisfaction: A persistent sense of dissatisfaction can overshadow accomplishments and enjoyment in life.
While there is a significant difference between MDD and Persistent Depressive Disorder, understanding these distinctions can provide insights into the daily challenge faced by individuals living with these disorders. Recognizing this can facilitate better support and treatment options tailored to each condition’s unique circumstances.
Treatment Approaches: What Works for Each Disorder
When evaluating the Difference Between MDD and Persistent Depressive Disorder, treatment strategies must be tailored to the specific disorder. Major Depressive Disorder (MDD) is often treated with a combination of medication and psychotherapy. Antidepressants such as SSRIs or SNRIs are frequently prescribed, helping to manage debilitating symptoms. In addition to medication, cognitive-behavioral therapy (CBT) is effective in addressing negative thought patterns, making it a common approach in the treatment of MDD.
On the other hand, Persistent Depressive Disorder (also known as Dysmythia) tends to require a more nuanced approach due to its chronic nature. Treatment often involves long-term psychotherapy, as individuals may benefit from establishing a therapeutic relationship over an extended period. Medication options can also include antidepressants, but the treatment may be supplemented with lifestyle changes and support groups to foster resilience. Recognizing the Difference Between MDD and Persistent Depressive Disorder is crucial for selecting the appropriate therapeutic interventions.
The Role of Therapy in Managing MDD and PDD
Therapy plays a critical role in the treatment of both Major Depressive Disorder (MDD) and Persistent Depressive Disorder (PDD), addressing the unique challenges associated with each condition. For individuals with MDD, therapy often serves as a vital resource for understanding triggers and developing coping strategies. This can include Cognitive Behavioral Therapy (CBT), which helps patients reevaluate negative thought patterns, or Interpersonal Therapy (IPT), which focuses on improving interpersonal relationships. Engaging in these therapeutic modalities fosters a supportive environment that encourages self-exploration and personal growth, integral in recognizing the difference between MDD and Persistent Depressive Disorder.
In contrast, those coping with PDD may benefit from a more long-term therapeutic approach, as symptoms can be pervasive and less intense but significantly impact daily life. Therapists often employ behavioral activation techniques to inspire greater engagement in enjoyable activities and reduce avoidance behaviors. Additionally, mindfulness-based therapies may provide individuals with tools to manage their feelings without becoming overwhelmed. Recognizing the difference between MDD and Persistent Depressive Disorder allows practitioners to tailor their therapeutic techniques, ensuring that each patient receives the most suitable form of support on their journey toward recovery.
Medication Options: Tailoring Treatment for Individual Needs
When exploring the Difference Between MDD and Persistent Depressive Disorder, it becomes evident that personalized medication options are crucial in addressing the unique profiles of individuals experiencing these conditions. Major Depressive Disorder (MDD) is often characterized by severe, episodic depressive episodes, whereas Persistent Depressive Disorder (PDD), previously known as dysthymia, entails a more lingering, chronic form of depression. Tailoring treatment to suit these differences can enhance efficacy and improve outcomes. Medications such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and atypical antidepressants may be employed, depending on the severity and nature of the symptoms.
For optimal results, a holistic approach that considers factors such as symptom duration, previous treatment responses, and personal preferences is essential when determining medication options. Below is a brief comparison of common medications suited for MDD and PDD:
| Medication Type | MDD Suitability | PDD Suitability |
|---|---|---|
| SSRIs | Effective for severe episodes | Can alleviate chronic symptoms |
| SNRIs | Good for pain-related symptoms | Useful for dual symptomatology |
| Atypical Antidepressants | Beneficial for resistant cases | May enhance mood stability |
Understanding the Difference Between MDD and Persistent Depressive Disorder is key to making informed choices regarding medication; this ultimately helps to mitigate any overlapping signs and symptoms effectively. Involving mental health professionals in this journey ensures a thorough assessment and optimal care plan tailored to individual needs, which may include psychotherapy or lifestyle modifications alongside medication. Establishing a support system and continuously evaluating the effectiveness of the chosen treatments allows for adjustments and improvements in managing depression.
Coping Strategies for Individuals with MDD and PDD
For individuals grappling with Major Depressive Disorder (MDD) or Persistent Depressive Disorder (PDD), various coping strategies can be pivotal in managing their symptoms and enhancing their quality of life. Engaging in mindfulness practices, such as meditation and deep breathing exercises, can help ground individuals in the present moment, countering the overwhelming feelings often associated with these disorders. Additionally, establishing a consistent daily routine fosters a sense of normalcy and predictability, which can be comforting amidst emotional turmoil. Other effective strategies include seeking social support from friends and family or joining support groups, where shared experiences can foster understanding and belonging.
It’s crucial to explore healthy lifestyle choices that contribute to improved emotional well-being for both MDD and PDD. Incorporating regular physical activity, such as walking or yoga, can boost mood through the release of endorphins. Fostering a balanced diet rich in nutrients also plays a crucial role in mental health. Furthermore, maintaining a sleep schedule is essential, as quality sleep can significantly impact overall mood and emotional stability. Below is a summary of strategies tailored to address the difference between MDD and Persistent Depressive Disorder:
| Strategy | MDD | PDD |
|---|---|---|
| Mindfulness Techniques | Highly Beneficial | Moderately Helpful |
| Regular Exercise | Essential | Helpful |
| Sleep Hygiene | Critical | Important |
| Social Connections | Vital | Supportive |
The Importance of Support Networks and Community Resources
In navigating the difference between MDD and Persistent Depressive Disorder, the role of support networks and community resources cannot be overstated. These groups provide emotional backing during challenging times, helping individuals to better understand their diagnoses and engage with treatment options. Finding a community, whether online or in person, with people who share similar experiences can be empowering. Supportive relationships create an environment where individuals feel safe to express their concerns, share coping strategies, and find hope amidst their struggles.
Access to community resources is equally vital in managing mental health conditions. Many organizations offer workshops, support groups, and educational materials that delve into the difference between MDD and Persistent Depressive Disorder. Such resources can clarify the nuances between these disorders, facilitating better self-awareness and recovery paths. Potential benefits of these networks include:
- Peer Support: Connecting with others facing similar challenges.
- Resource Sharing: Discovering helpful tools and strategies.
- Professional Guidance: Accessing mental health professionals for guidance.
- Community Activities: Engaging in activities that promote well-being.
Recognizing When to Seek Help: Guidance for Patients
Understanding the Difference Between Mdd and Persistent Depressive Disorder is crucial for individuals experiencing symptoms that affect their daily functioning. If you find yourself feeling persistently sad, hopeless, or unable to enjoy activities you once loved, it may be time to reach out for help. Here are some indicators that seeking assistance could be beneficial:
- Length of Symptoms: If you have experienced depressive symptoms for an extended period that seem unmanageable.
- Impact on Daily Life: Difficulty in carrying out day-to-day responsibilities, including work, school, or social interactions.
- Physical Symptoms: Experiencing changes in appetite, sleep patterns, or chronic fatigue.
- Loss of Interest: A noticeable decrease in enjoyment or interest in activities that used to bring you joy.
Recognizing these signs is pivotal in understanding the Difference Between Mdd and Persistent Depressive Disorder. Early intervention can significantly improve your quality of life. Here’s a quick reference table outlining when to consider professional help based on symptom duration and severity:
| Symptom Duration | Consider Seeking Help |
|---|---|
| Less than 2 weeks | Monitor and assess; may not require immediate help. |
| 2 weeks to 2 months | Consider seeking help if symptoms worsen. |
| More than 2 months | Seek professional help to explore the Difference Between Mdd and Persistent Depressive Disorder. |
Everyone experiences emotional struggles differently, and identifying when these emotions cross into the realm of needing professional support is essential. If you find yourself questioning how you differentiate between Mdd and Persistent Depressive Disorder, don’t hesitate to reach out to a mental health professional who can guide you through your journey.
Moving Forward: Hope and Recovery in Depression Management
Understanding the Difference Between MDD and Persistent Depressive Disorder is crucial for effective treatment and management. Major Depressive Disorder (MDD) is characterized by debilitating episodes of severe depression, which can last for weeks or months. During these episodes, individuals may find it challenging to engage in daily activities, feel persistent sadness, experience a loss of interest in things once enjoyed, or even exhibit changes in appetite and sleep patterns. The acute nature of MDD often requires immediate intervention and tailored treatment plans, including therapy and medication.
On the other hand, Persistent Depressive Disorder (PDD), historically known as Dysthymia, manifests as a chronic form of depression lasting for at least two years in adults. Individuals grappling with PDD might face a continuous low mood, but the symptoms are often less severe compared to MDD. Unfortunately, this prolonged experience can lead to significant impairment in daily functioning and quality of life. Recognizing the Difference Between MDD and Persistent Depressive Disorder empowers individuals to seek appropriate support and instills a sense of hope for those yearning for recovery. Below is a quick comparison to highlight the distinctions clearly:
| Aspect | Major Depressive Disorder (MDD) | Persistent Depressive Disorder (PDD) |
|---|---|---|
| Duration | Episodes last weeks to months | Chronic; at least 2 years |
| Severity of Symptoms | Severe during episodes | Milder but persistent |
| Treatment Approach | Immediate intervention often needed | Long-term management is essential |
The Difference Between MDD and Persistent Depressive Disorder signifies not just a clinical diagnosis but the unique experiences of those affected. Individuals facing either type of depression can benefit from shared stories and support networks. By fostering an environment of understanding and compassion, we can aid in the journey toward recovery, reminding every person that there is hope and healing available.
Frequently Asked Questions
Q&A: Understanding the Differences Between Major Depressive Disorder (MDD) and Persistent Depressive Disorder (PDD)
Q1: What is Major Depressive Disorder (MDD)?
A1: Major Depressive Disorder (MDD) is a mental health condition characterized by a persistent feeling of sadness or a lack of interest in outside activities. Symptoms often include significant weight changes, sleep disturbances, feelings of worthlessness, and difficulty concentrating. Episodes can last for a minimum of two weeks but may persist for months or even years without treatment.
Q2: How does Persistent Depressive Disorder (PDD) differ from MDD?
A2: Persistent Depressive Disorder, formerly known as dysthymia, is a chronic form of depression that lasts for at least two years in adults (one year in children and adolescents). While the symptoms of PDD are generally less severe than those of MDD, they can be more enduring. Individuals with PDD may experience episodes of MDD, but they also navigate a baseline level of depressive symptoms that can make daily life challenging.
Q3: What are the main symptoms of MDD and PDD?
A3: MDD symptoms include fervent feelings of sadness, hopelessness, and irritability, along with physical symptoms like fatigue, changes in appetite or sleep patterns, and difficulty making decisions. In contrast, PDD features a persistent low mood along with symptoms like low self-esteem and hopelessness, but without the more intense debilitating episodes typical of MDD.
Q4: Can someone have both MDD and PDD?
A4: Yes, it is possible for someone to experience both disorders. This is referred to as having a “double depression.” Individuals with PDD may have periods where they meet the criteria for MDD, illustrating the complex and nuanced nature of depression that can intertwine different forms.
Q5: How are MDD and PDD treated?
A5: Both MDD and PDD can be treated effectively through psychotherapy, medication, or a combination of both. Cognitive behavioral therapy (CBT) is commonly used for both disorders, while antidepressants like SSRIs may be prescribed for MDD and sometimes PDD. However, the treatment plan may vary based on the individual’s specific symptoms, duration, and intensity of the disorder.
Q6: How can someone distinguish between MDD and PDD?
A6: Distinguishing between MDD and PDD primarily lies in the duration and intensity of the symptoms. If one experiences severe symptoms that last for a minimum of two weeks, they may have MDD. If, however, the symptoms are chronic but less severe, persisting for two years or more, it would indicate PDD. A qualified mental health professional can provide an accurate diagnosis.
Q7: What would you recommend for someone struggling with these disorders?
A7: First and foremost, it’s important for individuals struggling with MDD or PDD to seek help from a mental health professional. Engaging in therapy, connecting with support groups, and discussing medication options can be vital steps toward recovery. Equally important is maintaining self-care, such as regular exercise, proper nutrition, and adequate sleep, which can play a significant role in managing symptoms.
Q8: Is awareness around MDD and PDD growing?
A8: Yes, awareness around both Major Depressive Disorder and Persistent Depressive Disorder has been growing, thanks to campaigns aimed at reducing stigma and advancing education on mental health. More people are recognizing the importance of discussing their feelings and seeking help, leading to a broader understanding of these conditions and their impacts on daily life.
Understanding the distinctions between MDD and PDD is essential in navigating the complex landscape of mental health. Whichever form of depression one faces, it is crucial to know that help is available and recovery is possible.
In Conclusion
understanding the difference between MDD and Persistent Depressive Disorder is crucial for proper diagnosis and treatment. While MDD involves episodic severe depression, Persistent Depressive Disorder presents a more chronic condition. Recognizing this difference between MDD and Persistent Depressive Disorder can help individuals seek appropriate support for their mental health needs.